In all living things, the skin represents the body’s first line of defense against external agents. The main function is protection against external chemical, physical and/or biological agents. It is able to produce antimicrobial peptides that limit bacterial and fungal infections, has immune-regulatory activity in limiting infections and neoplasms. Finally, it provides, with its flexibility, freedom of movement that would not otherwise be possible.
Among its innumerable functions are the production of vitamin D, protection from sunlight through the production of melanin (pigmentation), and thermoregulation. It is an important reserve source of water, electrolytes, vitamins, proteins and minerals; it also serves as a protection for the loss of the same (in/out action).
No less important is the function as a sensory organ by which we can perceive pain, itching, heat and cold. Without the skin, life would be impossible, and consequently the lack of even one of these activities implies the possibility of onset of both skin and systemic diseases.
For this organ to function perfectly, a barrier integrity is required, which is provided by multiple components: epidermis and dermis, hairs, and glandular adnexa.
Hairs have are an integral part of the defense system against pathogens and contribute to thermoregulation.
Sebaceous glands are essential in keeping the surface layer of the epidermis “soft and mobile” by secreting an emulsion of sebum; the latter spreads over the stratum corneum, moisturizing it; they provide an additional barrier against external pathogens. Sebum contains numerous fatty acids such as linoleic, oleic, and palmitic, which have antimicrobial activity.
The epitrichial sweat glands, on the other hand, ensure re-epithelialization of the skin surface and help, with the atrichial glands, with proper thermoregulation.
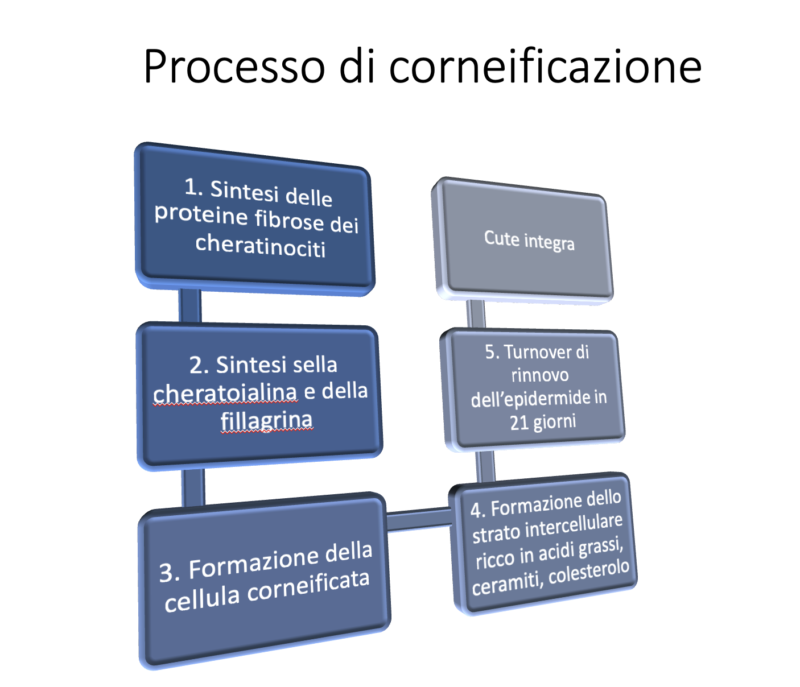
Finally, keratinocytes, the cells that form the skin barrier, accumulate keratin, lipids (e.g., cholesterol), fatty acids, and ceramides.
What happens if this complex structure does not function properly?
The intercellular lipid layer plays a key role in barrier integrity. A healthy dog has a turnover of corneocytes of about 21 days. Unlike in dogs with atopic dermatitis or some seborrheic diseases, this turnover is dramatically reduced to about 8 days.
Abnormal renewal of the epidermal layer promotes increased permeability to allergens, altered TEWL, and increased bacterial adhesion capacity. When keratinocytes break their cell wall and become corneocytes, they release certain elements that are essential for the integrity of the skin barrier. Specifically we can have an emulsion of albumins, complement, lipids, transferrin, sodium chloride, interferons. Some of these elements contribute significantly to preventing the increased adhesion of yeast bacteria of the genus Malassezia, such as transferrin, thus ensuring the “health” of the skin.
The epidermis itself, in its integrity plays an important role as the first immune defense against many pathogens (e.g., bacteria, fungi, etc.) by producing cytokines and chemokines, antimicrobial peptides. Corneocytes are also capable of producing pro-inflammatory agents such as GMCSF (granulocyte macrophage colony-stimulating factor), IL-8, TNF-alpha (tumor necrosis factor) against allergens such as Der F1(Dermatophagoides farinae 1) and/or lipopolysaccharides (these stimulate both local and systemic inflammatory response). Thus, corneocytes and keratinocytes do not represent a defenseless surface layer, but on the contrary, the first effective defense against external pathogens.
TEWL: How does skin dehydration worsen clinical symptoms of allergic disease?
Trans Epidermal Water Loss or TEWL represents the outflow of water from the skin and ensures normal skin homeostasis. In this particular balance, the stratum corneum represents a fundamental support for its perfect function. As mentioned earlier, the integrity of this layer serves to insulate from external agents, regulate water leakage, and control proper desquamation, proliferation, and differentiation of the epidermis.
Corneocytes and the TEWL
Corneocytes are keratinized keratinocytes joined together by a lipid intercellular matrix composed of approximately 50 percent ceramides, 10 percent fatty acids, 25 percent cholesterol, 15 percent cholesterol, and glycosylceramide derivatives. Ceramides, complex lipids formed from a sphingoid base linked to saturated fatty acids, are divided into 6 main classes, differing depending on the sphingoid and the length and hydroxylation of the respective saturated fatty acid chain; they can be either amphophilic or hydrophilic, and bind with other lipid components to maintain barrier integrity.
The most important fatty acids, which are essential for corneocyte bonding, are linoleic and gamma-linolenic. These bind to the intercellular lipid lamellae with ceramides, providing structure stability and regulating water evaporation from the skin.
Finally, cholesterol has the function of improving the plasticity and/or increasing the stiffness of lipid lamellae. It also maintains lipid barrier stability with the other components.
In recent times it has been seen that another component is also critical for maintaining barrier function: phyllagrin. This is synthesized in the granule layer and contributes to the formation of the corneified envelope together with lorichin. Together they help maintain thehydration of the more superficial layers of the skin.
What about in atopic dogs?
In atopic dogs, the barrier is not intact because we have an altered ratio of ceramides to cholesterol, a decrease in fatty acids: these abnormalities allow an alteration of normal cell turnover and desquamation, increased water loss, and a consequent increased passage of allergens or pathogens. Not least, dehydration and alteration of the skin barrier leads to skin dysbiosis with lower microbial biodiversity. It has been seen that dogs with atopic dermatitis have 3 times higher TEWL values than healthy dogs, and 2 times higher than those with the disease in remission (dogs on maintenance therapy).

The clinical consequence of a defective skin barrier is initially manifested in increased skin dehydration and increased susceptibility to secondary microbial infections (e.g., pyoderma). The passage of allergens, combined with skin dryness, promotes the triggering of a local immune response that will lead to erythema, itching and then a progressive worsening of skin lesions in sick dogs.
Skin dysbiosis and intestinal dysbiosis in atopic dogs

In recent years, studies inherent in the skin and intestinal microbiota have increased in relation to their role in defending the body. A healthy skin microbiota is critical for the maintenance of normal protective functions of the skin, an effective immune response to external pathogens, and the prevention of colonization by pathogenic microorganisms.
Dogs with atopic dermatitis have significant skin dysbiosis with a decreased diversity of resident bacteria. It is still not entirely clear whether the manifestation of allergic disease can be attributed to skin dysbiosis or whether this is a consequence of the disease. However, it is certain that the altered structure of the skin barrier can promote greater adhesion of bacteria to corneocytes and promote the occurrence of bacterial skin infections. Pyoderma in turn triggers an inflammatory process that is clinically manifested by erythema, papules, pustules, epidermal collaterals, and self-traumatic lesions and results in further worsening of TEWL. A vicious cycle is then triggered with recurrence of lesions, increased dehydration and skin dysbiosis. Equally, a healthy gut microbiota is necessary for the proper functioning and integrity of the intestinal barrier, as well as the regulation of the enteric immune system. As with the skin, this internal barrier protects against the proliferation of enteropathogens and ensures the prefect functioning of nutrient absorption capabilities. These two “in and out” systems are connected, and it has been seen that there is a close correlation between gut dysbiosis and allergic skin diseases such as atopic dermatitis.
Gut dysbiosis can promote increased enteric permeability to trophoallergens and aeroallergens inducing worsening of allergic disease. In fact, all atopic dogs, in addition to skin dysbiosis, have severe enteric dysbiosis. It is normally thought that if the animal’s feces are well formed, with a Fecal Score of 1-2 and negative for endoparasites, this is a clinical parameter indicative of intestinal well-being. In contrast, recent studies using gut microbiota analysis of atopic dogs have shown that they are all dysbiotic, regardless of diet, severity of dermatologic disease, and type of systemic medical therapies in place. Hence the need to adopt a strategy to restore skin and intestinal eubiosis.
Nutraceuticals to support restoration of skin integrity: use of fatty acids, natural anti-inflammatories and trace elements
The extracellular lipid matrix in which corneocytes are suspended is highly specialized and complex. In particular, the presence of the correct amount of linoleic acid is critical for the integrity of the barrier. This binds with ceramides contributing to proper skin hydration.
Generally, proper nutrition is sufficient in healthy animals to maintain normal skin balance. In domestic carnivores, the enzyme delta-6-desaturase is absent in the skin, and it is deficient or inefficient in the liver: in fact, polyunsaturated fatty acids cannot be synthesized by the body and must be taken in adequate amounts by the body.
In atopic dogs, the skin barrier is deficient in fatty acids, ceramides, and cholesterol, and normal nutrition is not sufficient to restore its balance. Numerous studies have been conducted to understand whether oral supplementation is sufficient to decrease TEWL and associated skin inflammation. A diet rich in omega 3 and omega 6 essential fatty acids in a ratio of 5:1 for at least 8 weeks was found to contribute to better organization of the lipid lamellae of the stratum corneum in atopic dogs. Equally other studies have shown that omega 6 and 3 in a ratio of 4:1 are the most effective in decreasing the formation of inflammatory leukotrienes (e.g., LTB 4). They act by interfering with the inflammatory cascade by producing PGE1, which goes against the formation of free arachidonic acid and prevents the formation of inflammatory leukotrienes such as LTB4. Decreased LTB4 formation leads to decreased neutrophil chemotaxis effect, limits the release of thromboxanes and inflammatory prostaglandins.
Clinically, there is a decrease in skin inflammation and erythema associated with allergic disease. Not to be forgotten, essential fatty acids have a “steroid sparing” effect, which is useful in decreasing doses of systemic cortisone as an anti-inflammatory.
Nutrition alone is not sufficient to control the disease; proper and consistent supplementation with fatty acids in the diet as a nutraceutical helps to partially restore the normal protective functions of the skin barrier.
Oral supplementation of essential fatty acids is often combined with trace elements and vitamins. It has been seen, for example, that zinc deficiency can mimic or even exacerbate the symptoms of essential fatty acid deficiency. Similarly, vitamin E can help decrease clinical signs of allergic skin diseases. This vitamin, found in cell membranes, has an excellent antioxidant effect and protects cell membranes from free radicals by preventing lipid peroxidation. Atopic dogs the level of vitamin E is lower than healthy dogs. Again, it has been seen that oral supplementation can help decrease skin inflammation and clinical symptoms.
In the group of natural anti-inflammatory agents are aliamides, lipid endocannabinoids, such as palmitoylethanolamide. These are able to reduce the release of pro-inflammatory chemokines and decrease mast cell degranulation. Although they do not act directly on the skin barrier as fatty acids do, they do induce a decrease in inflammation related to allergic disease; as a consequence for the same less inflammatory process, there is a decrease in TEWL.
What about gut dysbiosis?
It is crucial to remember that atopic dogs also have intestinal dysbiosis, which also necessitates supplementation with pro- and prebiotics, as well as parabiotics.
These are often found in oral nutraceuticals rich in fatty acids, particularly Lactobacillus rhamnosus is supplemented. This is able to regulate part of the immune system by modifying the inflammatory process a Th1-type cell-mediated response, with decreased itching. Other lactobacilli such as L. paracasei K71 or L. sakei have similar functions.
Clearly, a balanced diet is sufficient to ensure animal well-being in healthy individuals, but in dogs with atopic dermatitis this is often not: oral supplementation with ad hoc nutraceuticals is essential to ensure better control of the disease.
Topical therapy to restore normal skin balance: limitations and possibilities
In veterinary dermatology, the use of topicals supports the management of allergic diseases and can be formulated in shampoos, emulsions, foams, and spot ons. These preparations are used as a vehicle for moisturizing, barrier restructuring, or antiseptic substances. Moisturizers, emollients and humectants are indicated to restructure the skin barrier. Moisturizers include glycerol and urea, alone or in combination with fatty acids, ceramides, or other elements such as biotin.
The main emollients, on the other hand, have a lipid component and can be paraffin-based or mineral oils, lanolin, fatty acids with natural antioxidants (e.g., Vit A or E). There are also non-lipid component ones containing lactic acid, propylene glycol and urea.
Shampoo may become an important therapy in the multimodal management of canine atopic dermatitis because of its specific characteristics: it removes dirt and allergens, moisturizes the skin, and may have antiseptic activity. There are many good quality products on the market often in combination with phytotherapeutics. Frequency of use and type of product differ according to the severity of dermatological lesions and adherence of owner and dog. Some dogs resent bathing, and some owners are unable to perform the therapy properly due to lack of time or a suitable place (e.g., bathtub for large dogs).

Where possible, this treatment can also be performed 2-3 times a week, but it is generally weekly. Shampoo therapy is a “therapy” and therefore differs from normal dog hygiene. The purpose is to moisturize and restructure the skin barrier, decrease inflammation and possibly take advantage of antiseptic activity.
As much as shampooing is an integral part of treatment of allergic diseases, it can be counterproductive in some individuals. In particular, products with antiseptics (e.g., chlorhexidine), if not rinsed well, can cause contact dermatitis and erythema, resulting in worsening of the main disease. The pH must also be appropriate for the dog’s skin, which on average has values between 5.5 and 7.2: formulations that are too acidic or too basic are therefore unsuitable (e.g., dermatological shampoos for human use).
Other products can be similarly useful, where we have limited injuries, in spray. Spot-on moisturizers have found an interesting application in recent years. The mechanism exploited is similar to that of “pipette” pesticides: you apply the product on the back and it spreads evenly over the trunk. These preparations are easy to use and effective, but they cannot replace shampoo therapy, which has the added benefit of warding off dirt and allergens.
Recently introduced topical sprays with tindalized lactobacilli (e.g., Lactobacillus rhamnosus, Lactobacillus reuteri) and plant polyphenols to support the skin microbiota. The skin microbiome also contributes to normal barrier function, and the new products complement the concept of “in/out” management of allergic disease.
Recommended readings
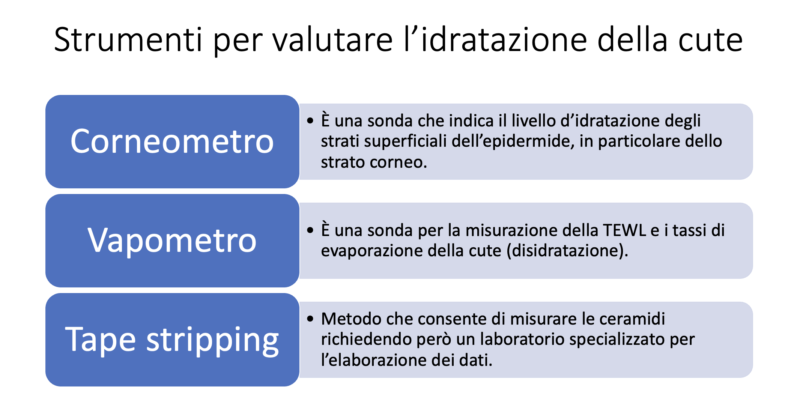
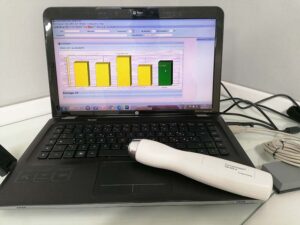
- Cobiella D, Archer L, Bohannon M, et al. Pilot study using five methods to evaluate skin barrier function in healthy dogs and in dogs with atopic dermatitis. Veterinary Dermatology 2019, 30: 121-e34. doi.org/10.1111/vde.12723.
- Cornegliani L, Persico P, Di Prinzio R, et al. Valutazione del microbiota intestinale in cani sani e cani affetti da dermatite atopica cronica. Veterinaria 2021, 35 (4). In press.
- Marsella R. Advances in our understanding of canine atopic dermatitis. Veterinary Dermatology 2021, doi.org/10.1111/vde.12965.
- Nuttal TJ, Marsella R, Rosenbaum MR, et al. Update on pathogenesis, diagnosis, and treatment of atopic dermatitis in dogs. Journal of the American Veterinary Medical Association 2019, 254:1291-1300.
- Padmanabhan N, Krishnamoorthy G. Therapeutic relevance od dietary ratio of polinsatured fatty acids N6:N3 in canine atopic dermatitis. EC Nutrition 2017, 9: 36-50.
- Watson A, Thomas G, Butowski C, et al. Evidence for an interaction between linoleic acid intake and skin barrier properties in healthy dogs. A pilot study. Journal of Applied Animal Nutrition, 2018: 6: 1-5.
- Zajac M et al: assessment of the relationship between transepidermal water loss (TEWL) and severity of clinical signs (CADESI-03) in atopic dogs. Veterinary Dermatology 2014; 25: 503-e83.







