The skin barrier disruption found in atopic dermatitis (AD) is linked to increased water loss and a possible increase in allergic sensitization. In humans, numerous studies have demonstrated the effectiveness of emollient or moisturizing creams in restoring the barrier, and this approach has been the mainstay of AD therapy for years. And, recently, this strategy has also shown promise as a preventive option.
Whether restoration of the skin barrier is equally effective and directly results in improved clinical signs in the dog with AD is, however, yet to be clarified.
In Veterinary Dermatology Rosanna Marsella, of the College of Veterinary Medicine, Florida, USA, compared what is currently known about the options used to repair the skin barrier in human and veterinary medicine.
Human DA: what is the best choice
The importance of addressing skin dryness in humans with atopic dermatitis has been known for decades. There is a direct relationship in such patients between disease severity and dryness of the skin, in which abnormalities of both lipids (e.g., ceramides) and proteins (e.g., filaggrin) have been described. Some alterations are genetically inherited (such as filaggrin mutations, which are a major risk factor of AD), while others are secondary and related to inflammation.
Reviewing the different options to date, the author points out that:
- both moisturizing and emollient creams have been shown to improve the skin barrier and clinical signs;
- “barrier creams” increase the time between flare-ups and reduce relapses by about one-third compared with no treatment;
- topical therapy with glucocorticoids or calcineurin inhibitors is an option that has proven successful, inducing disease remission in humans in both cases, accompanied by improvement of the skin barrier;
- skin care also has a preventive function. Early implementation of emollient (Vaseline-based) therapy reduces the frequency of AD development in high-risk children to 15%, compared with 30-50% when no skin care is performed.
Despite the fact that skin barrier repair has been practiced for a long time, however, the debate about the best ingredient to use is still ongoing. In fact, it was seen that:
- water-based moisturizing lotions and humectants in the long run may contribute to the breakdown of the stratum corneum, opening it to water evaporation (TEWL, TransEpidermal water loss); therefore, lipid-based emollients, such as rich ointments and creams, seem to be preferred in the treatment of atopic dermatitis;
- The most commonly used ingredients for skin repair are: petrolatum (Vaseline), vegetable oils, glycerin and urea; the choice of composition is crucial in the long run
- barrier creams based on ceramides, cholesterol, and fatty acids have been approved in recent years and have shown comparable efficacy to fluticasone-based creams;
- a combination of plant extracts, including glycyrrhetinic acid and Vitis vinifera extract have shown antipruritic properties.
But a recent study comparing all three showed no significant differences in effectiveness, fueling the debate.
- Both steroid therapy and calcineurin inhibitor therapy control inflammation and reduce TEWL, but only the latter appear to be able to repair the stratum corneum, standing as a candidate as the most appropriate approach for long-term therapy in terms of maintaining the skin barrier.
Therefore, it seems that more and larger controlled studies are needed to address the question of which approach for skin repair is clinically most effective and whether this can also be used as a preventive strategy.
What is known in dogs
In agreement with findings in humans, there is skin barrier dysfunction in canine AD, which may increase the risk of allergic sensitization. Decreased ceramides and abnormal ultrastructure of the stratum corneum have been described. An increase in glucosylceramides, free and protein-bound, then suggests a defect in ceramide metabolism, and finally, a significant decrease and altered metabolism of sphingosine-1-phosphate in injured atopic skin compared with healthy skin has been described.
All these findings underscore the importance of exploring skin barrier repair in veterinary medicine.
Lack of reliable evaluation methods
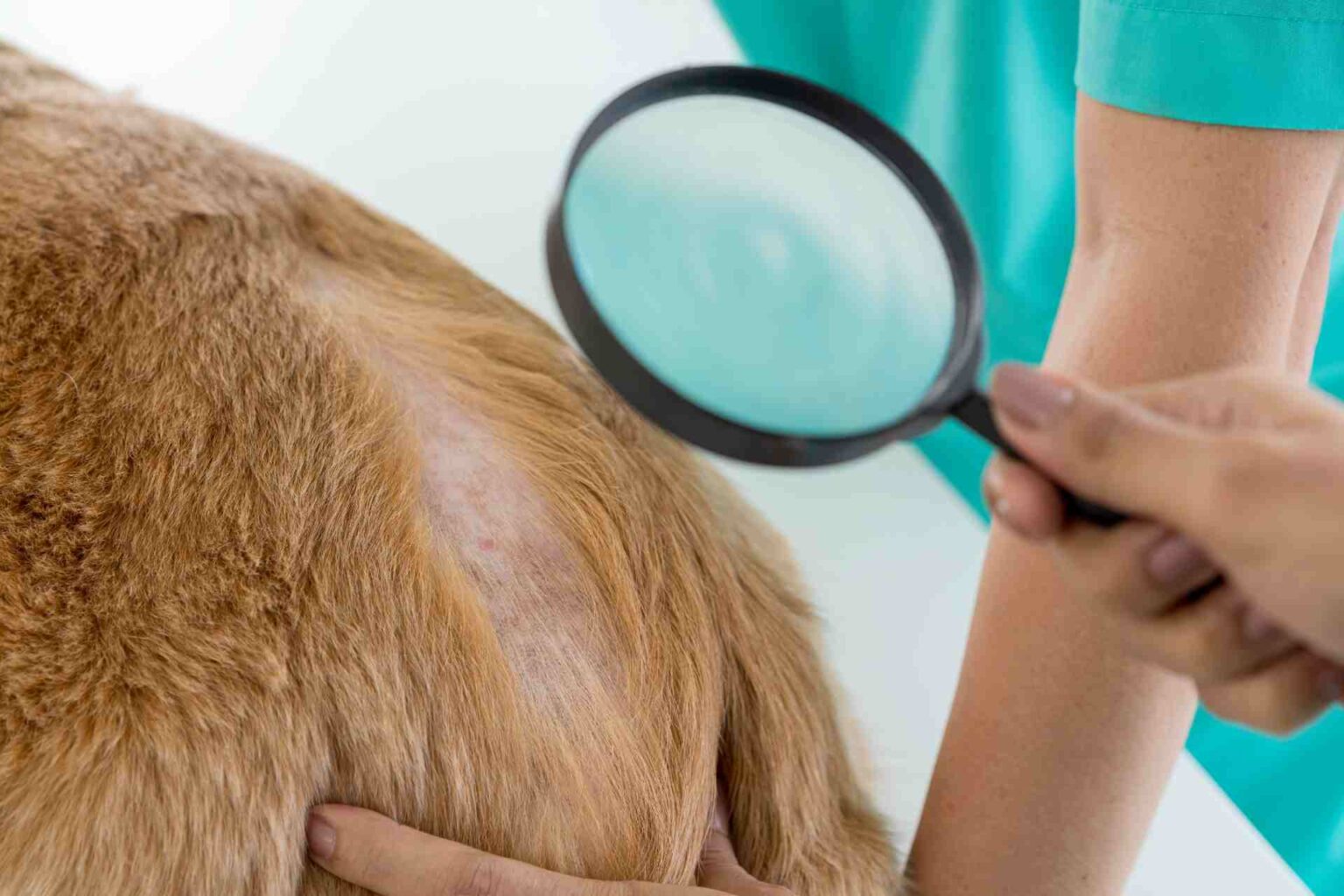
In dogs, the skin barrier is often assessed by TEWL, although the reliability of this methodology is not good.
There is a relationship between ceramide deficiency and increased TEWL, but a relationship between disease severity and skin barrier dysfunction as measured by TEWL has yet to be demonstrated.
The lack of significant improvement in TEWL may be an indication of poor reliability of TEWL measurements rather than the lack of skin barrier improvement in light of ultrastructural studies.
Furthermore, while it is reasonable to assume that restoration of lipid deficiency improves skin barrier function, it is yet to be ascertained whether barrier repair can directly translate into improved clinical signs.
Reviewing the published comments in the veterinary field here is the evidence.
Products rich in lipids/ceramides
- The topical application of products containing Ceramides, free fatty acids and cholesterol improves stratum corneum ultrastructure and increases the number of interlamellar lipids, but the demonstration of clinical benefit is still limited: an open study in dogs with chronic AD showed a clear improvement in erythema, but the number of subjects was small and a control group was missing. A double-blind, placebo-controlled study reported a significant decrease in clinical signs compared with the control group, although results on TEWL were mixed.
- An open study with products containing essential oils and unsaturated fatty acids also showed a significant decrease in clinical scores and itching, but without showing any improvement in TEWL.
- Oral administration of omega-6 and omega-3 fatty acids, mixed 5 : 1 (v ⁄ v); improved ultrastructure and increased lipid content in the skin of atopic dogs, but correlation with clinical improvement was lacking.
- There is currently a lack of evidence to support the topical application of phytosphingosine because a study that compared a shampoo that contained it with two other treatments with emollients or medicated shampoos-all theoretically capable of improving the skin barrier-could not demonstrate an extra benefit of sphingosine over the other treatments. No assessment of skin barrier function was performed in this study.
Barrier creams and other strategies
- “Barrier creams” or skin protectants (e.g., dimethicone) provide an exogenous barrier to water loss, but although this may be an effective and inexpensive strategy, a double-blind placebo-controlled study failed to demonstrate improvement in clinical signs and TEWL.
- Ultrapure fresh water has beneficial effects on the skin barrier compared to tap water and has decreased itching and dermatitis scores.
Glucocorticoids, calcineurin inhibitors, and allergen-specific immunotherapy
- Oral prednisolone in dogs with AD failed to report a superior effect compared with cyclosporine for TEWL. Clinical signs improved in both groups, but TEWL was not correlated with clinical improvement.
- In contrast, successfulallergen-specific immunotherapy was correlated with decreased TEWL compared with atopic dogs that did not respond to allergen-specific immunotherapy.
Conclusion
“Skin barrier repair is a promising, but as yet under-explored,approach to the management of canine AD ,” she points to conclude, “and could prove very beneficial when initiated early in life, improving the course of AD and minimizing the development of allergic sensitization.
However, larger controlled studies exploring what is the best treatment and long-term effects on the skin barrier are lacking because choosing the wrong ingredients could have long-term adverse effects and eventually worsen an already compromised skin barrier.
Reference
Marsella R. Fixing the skin barrier: past, present and future – man and dog compared. Vet Dermatol 2013; 24: 73–e18
DOI: 10.1111/j.1365-3164.2012.01073.x